Information (McDougall Team or Programs)
Filter by:

John McDougall, MD: Announcement of Retirement
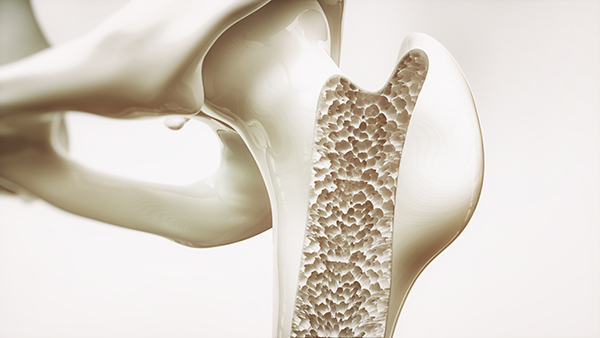
Osteoporosis: The Truth About Women’s Bone Health

The Food Elimination Diet: What You Need to Know
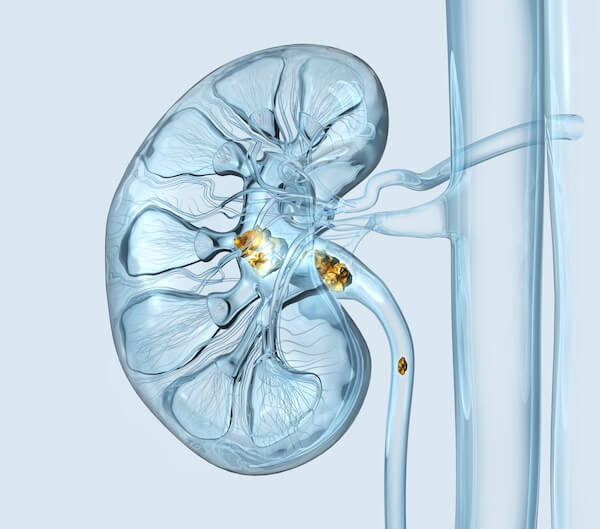
The Truth About Oxalates & Kidney Stones

Ozempic – A Miracle Weight Loss Drug Mimicking Sickness
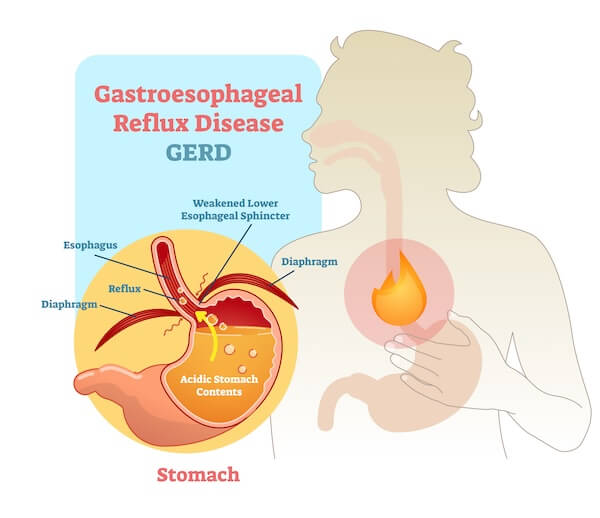
My Stomach’s on Fire and I Can’t Put it Out
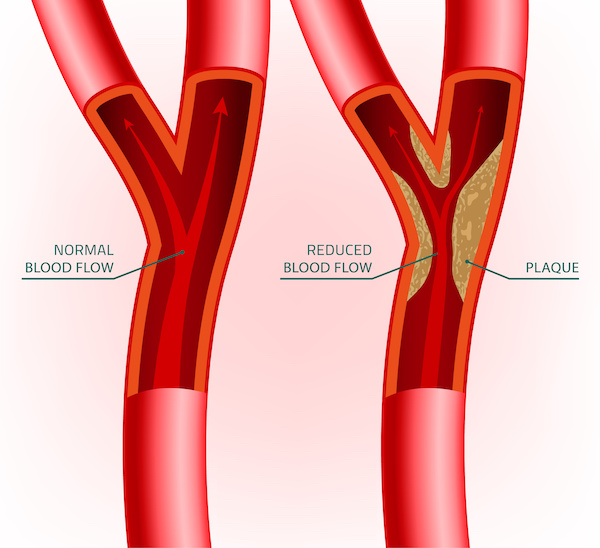
Cleaning Out Your Arteries

In Search of the Perfect Bowel Movement – Part 1

Stocking Your Kitchen
Protein Overload
An Insider’s View of the 12-Day McDougall Program






