Paula: Cured Endometriosis
Diet Cured My Endometriosis and Helped Me Have My Son
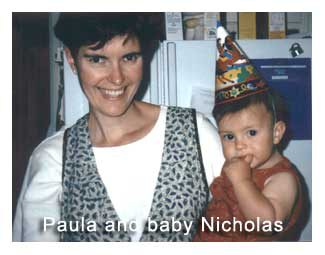
Because of the McDougall Program I was able to rid my body of a painful chronic female condition, endometriosis, that causes suffering and infertility for millions of women, and eventually have a baby.
I went through menarche in 1971 at the age of 13 and from my first period, I had severe dysmenorrhea, the medical term for menstrual cramps. With each subsequent menstruation the cramps got worse. By the time I attended college, the dysmenorrhea was so debilitating I spent the whole first day of my cycle in bed with a hot pack and a “barf bowl” nearby because the severe pain caused me to throw up.
The doctors I saw while I was in high school and college suggested that with more exercise I might feel better. However, I was already riding my bike 6-15 miles a day, taking ballet 5 mornings a week, swimming on the high school swim team, and playing tennis 2 times a week. I wasn’t sure what more exercise I could do. I took up Yoga because one doctor told me it might help. It was fun, but didn’t help the menstrual cramps. At this time I was 5’8″ and 112 lb. and appeared to be the picture of good health to those around me.
I did get some temporary pain relief with Darvocet and alcohol, though I’d often throw this combination up also. When the first anti-prostaglandin drug, Ponstel (a NSAID), came out in the late 70’s I tried it, but I only got mild and temporary relief—I still couldn’t function well enough to leave the house on the first day of my cycle.
In my 20’s I started trying to have a baby. Many people, including medical doctors, assured me that the cramps would improve after giving birth. But of course, I couldn’t conceive. In 1987, at the age of 29, I had a laparoscopy by an infertility specialist to find out the cause. He diagnosed me with endometriosis. This specialist, who had performed hundreds of similar surgeries, told me I had the worst case of this female inflammatory disease he had seen in someone in their 20’s. He removed some of the endometrial tissue that he could see through his scope, but explained that surgery alone could not cure the condition. I needed medication to stop my menses so that my body could heal. I started on Danocrine (a male-like hormone) after surgery, but I had to stop it after only 10 days due to the side effect of severe depression.
Next I was offered an experimental injectable drug, Lupron, which is used to decrease the body’s production of both male and female hormones and is commonly prescribed for the treatment of prostate cancer. I decided that even if I never got pregnant, just being free of the dysmenorrhea was worth trying the new drug. I received an injection once a month for 6 months, and promptly went into menopause, complete with hot flashes. Even after stopping the Lupron, I remained in menopause for an additional 6 months.
A year later, when I started menstruating again, my husband and I, wanting to have children, sought the help of an infertility specialist The specialist told me I probably wouldn’t conceive without the help of in vitro-fertilization. In the 80’s the process had only a 25% success rate, and cost close to $10,000 per try. We decided that we didn’t want a baby that badly. I was just happy to be free of the menstrual cramps. But the dysmenorrhea returned! Within 6 months of resuming menstruation, I was back to spending the first day of my cycle in bed, and desperate for any pain medication I could procure.
My turning point came in 1991, when my vegetarian sister sent me a copy of The McDougall Plan (originally published in 1983). I had been a lacto-ovo vegetarian since reading Diet for a Small Planet at 16 years old, and though I ate no meat I ate copious amounts of dairy products. Dr. McDougall’s instructions were simple: eat a diet based on starches with the addition of fruits and vegetables, and eliminate all sources of dairy from your diet. I stopped consuming milk, butter, ice cream, yogurt & cheese, and as instructed, eliminated all crackers and other products containing whey and casein. For good measure, I stopped eating eggs as well. My family worried I would get sick, but I figured I was already sick. I had nothing to lose.
The changes started in about 4 months; I started having less severe pain with my menses. By 8 months after eliminating dairy, I no longer had any dysmenorrhea at all, something I had never experienced since puberty. I was thrilled. I had forgotten about trying to get pregnant. I was just happy to be free from pain! But then a miracle happened. Two years after eliminating dairy, at the age of 35, I spontaneously got pregnant without assistance from an infertility specialist. I was so amazed, I went to visit the infertility MD to show him what had happened. He congratulated me but then warned me that I might not want to tell many people I was pregnant—because of the severe scarring from the endometriosis, I was likely to have a miscarriage.
So I told only close friends and family that I was pregnant, and continued to follow the McDougall vegan diet. When the pregnancy progressed to a point where I could no longer hide it, I admitted to people that yes, I was expecting a baby. And when I told them why—my change in diet—they wouldn’t believe me. Many people cautioned me about eating a vegan diet while pregnant. Many others, my midwife included, wanted me to take supplements to assure a healthy baby. But I figured this diet enabled me to get pregnant in the first place, I best stick with it. I politely refused the supplements, getting what I needed in the way of nutrition from food. I didn’t even take B12 because I decided my stores were probably adequate. I did start eating walnuts at the suggestion of the perinatologist at work, because she believed they contained something crucial for brain development, and I ate greens daily for the folate.
Nine months later, my healthy 7lb. 12oz son was born on his due date at our home in Manhattan Beach, CA. The uneventful delivery was attended by two nurse-midwives. My blood loss at delivery was so minimal they joked that it was the cleanest delivery they had seen in a while. The only effect we noticed from the endometriosis scarring was that I had a tearing sensation across my abdomen while pushing. A hot pack took care of the pain, and allowed me to push the baby out. I never felt like I needed medication for the pain in labor. Interestingly, labor pain was easy compared to the dysmenorrhea I’d had with my menses.
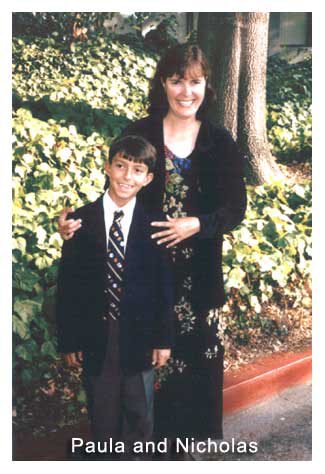
Of course, I’ve raised my son as a vegan. He is a healthy child, whose first and only ear infection was in 2nd grade after being introduced to cow’s milk ice cream at school. He is 10 1/2 years old now, in the 90th percentile for height and 65th percentile for weight. He’s very athletic, smart and very rarely sick. Over the years, my son has remained a vegan, though like many children his age, he doesn’t consume enough fruit and vegetables to please his mother.
I have toyed with the idea of adding meat & fish to my diet. I’ve found at conferences and when traveling that classifying myself as a vegetarian often prompted meals that contained dairy. Since I wanted to avoid dairy, I often chose a meat dish. After doing that for the last 4 years, I’ve gained close to 20 lb., at a rate of 5 lb. a year. This last year I decided it was time to go back to being vegan again, and without difficulty the weight is slowly melting off. Attending the VegSource Expo this last October, 2005 gave me the chance to meet Dr. McDougall in person and thank him belatedly for his role in helping me become pain free and a mother. His only request of me was to share my story so others could be helped.
Dr. McDouall’s Comments:
Endometriosis is one of the most common gynecological problems affecting an estimated 5.5 million women in North America, but this condition may occur at a subclinical level in half of all women following the Western diet, as discovered by autopsy.1 This disease occurs when the endometrial tissues lining the inside of the uterus spread outside of the uterus and become attached to the ovaries, fallopian tubes, the bowels and other internal abdominal parts. This misplaced endometrium responds to the menstrual cycle in the same way as the original tissues of the uterine lining: each month the tissues build up, then break down, and shed. In the abdominal cavity the internal bleeding results in inflammation, causing pain, infertility, scar tissue formation, adhesions, and bowel problems.
Every scientist and doctor agrees that the cause and course of endometriosis involves female reproductive hormones. However, few of these experts know about the connection between hormones, endometriosis, and diet—but they should. Studies of populations of women show the risk of developing endometriosis is much higher with the consumption of red meat and beef, and much lower with consumption of vegetables and fruits.2 A similar dietary connection is found with other diseases of the female reproductive organs, including uterine fibroids, ovarian cysts, and cancers of the uterus (endometrium) and ovary.2-6
The rich Western diet changes female hormones and as a result causes the development of disease in tissues that are hormone dependent—those of the uterus, ovary, vagina, and breast. Environmental chemicals, lack of dietary fiber, excess dietary fat, estrogens in cow’s milk, lack of plant-derived phytoestrogens, and resulting obesity are some of the means by which diet adversely affects hormones.6-10 Most importantly, when a woman changes to a low-fat, plant-food based diet her reproductive hormones correct and most troublesome female problems, like heavy menstrual bleeding, fibrocystic breast disease, and PMS are alleviated. Her risk of future health problems such as breast and uterine cancer are also greatly reduced.
Too little research has been done on fertility and diet but, what is known is that a low-fat diet and/or weight loss will improve the function of the ovaries and reproductive qualities of a woman.11-12 Clearly, this Star McDougaller’s experiences attest to the health and reproductive benefits of a low-fat plant-food-based McDougall diet.
Paula showed great courage by following a non-traditional diet while pregnant, and then raising her son as a vegan. Hardly a dietitian or doctor in the entire world would have supported her, but she was right—the best diet for a pregnant woman and a growing child is the McDougall Diet (vitamin B12 is recommended). Anyone willing to open their eyes can see that the dairy- and meat-laden Western diet is at the root of the epidemic of obesity and sickness that plague people young and old, even those with child. Unfortunately, diet seems to be the last remedy anyone tries—after all the modern miracles from the medical and pharmaceutical industry have failed.
![]()
- Williams TJ, Pratt JH. Endometriosis in 1,000 consecutive celiotomies: incidence and management. Am J Obstet Gynecol. 1977 Oct 1;129(3):245-50.
- Parazzini F, Chiaffarino F, Surace M, Chatenoud L, Cipriani S, Chiantera V, Benzi G, Fedele L. Selected food intake and risk of endometriosis. Hum Reprod. 2004 Aug;19(8):1755-9.
- Chiaffarino F, Parazzini F, La Vecchia C, Chatenoud L, Di Cintio E, Marsico S. Diet and uterine myomas. Obstet Gynecol. 1999 Sep;94(3):395-8.
- Levi F, Franceschi S, Negri E, La Vecchia C. Dietary factors and the risk of endometrial cancer. Cancer. 1993 Jun 1;71(11):3575-81.
- Bosetti C, Negri E, Franceschi S, Pelucchi C, Talamini R, Montella M, Conti E, La Vecchia C. Diet and ovarian cancer risk: a case-control study in Italy. Int J Cancer. 2001 Sep;93(6):911-5.
- Rock CL, Flatt SW, Thomson CA, Stefanick ML, Newman VA, Jones LA, Natarajan L, Ritenbaugh C, Hollenbach KA, Pierce JP, Chang RJ. Effects of a high-fiber, low-fat diet intervention on serum concentrations of reproductive steroid hormones in women with a history of breast cancer. J Clin Oncol. 2004 Jun 15;22(12):2379-87.
- Bagga D, Ashley JM, Geffrey SP, Wang HJ, Barnard RJ, Korenman S, Heber D. Effects of a very low fat, high fiber diet on serum hormones and menstrual function. Implications for breast cancer prevention. Cancer. 1995 Dec 15;76(12):2491-6.
- Woods MN, Barnett JB, Spiegelman D, Trail N, Hertzmark E, Longcope C, Gorbach SL. Hormone levels during dietary changes in premenopausal African-American women. J Natl Cancer Inst. 1996 Oct 2;88(19):1369-74.
- Ganmaa D, Sato A. The possible role of female sex hormones in milk from pregnant cows in the development of breast, ovarian and corpus uteri cancers. Med Hypotheses. 2005;65(6):1028-37.
- Rier SE. The potential role of exposure to environmental toxicants in the pathophysiology of endometriosis. Ann NY Acad Sci. 2002 Mar;955:201-12;
- Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Protein intake and ovulatory infertility. Am J Obstet Gynecol. 2008 Feb;198(2):210.e1-7.
- Wilkes S, Murdoch A. Obesity and female fertility: a primary care perspective. J Fam Plann Reprod Health Care. 2009 Jul;35(3):181-5.
Recommended Articles

Syd Wyemann: My Hands Were Crippled With Arthritis

Manuela: Weight, High Blood Pressure, High Cholesterol and Kidney Stones are a thing of the past thanks to The Starch Solution!







