Results of the Diet & Multiple Sclerosis Study
Updated July 31, 2014
On Tuesday, January 16, 2008 the McDougall Program made first contact with the Department of Neurology at Oregon Health & Science University (OHSU, the medical school in Portland, Oregon) with a proposal to study the effects of a very low-fat diet on Multiple Sclerosis (MS). OHSU was chosen because of Roy Swank, MD, head of the Division of Neurology at OHSU from 1954 until 1974. Dr. Swank was the founder of the low-fat dietary approach to MS. He was also my friend and one of my mentors.
During his remarkable career Dr. Swank published dozens of studies in major medical journals showing that a low-fat diet would essentially stop the progression of MS. Unfortunately, his work never caused an impact on the practice of neurology, primarily because there is no financial incentive to promote simple diets to cure diseases. Drug therapies, costing $55,000 annually, are the only therapies available to MS patients, even though they are largely ineffective. With the best efforts of well-meaning neurologists, half of patients diagnosed with MS will become severely disabled, or worse, within 10 years.
The excuse medical doctors use for ignoring Dr. Swank’s cost-free, side effect-free approach is that his studies of 5,000 patients spanning 50 years of research were observational. “Real scientists” preach a gold standard of research called, the doubled-blind, randomized, placebo-controlled trial. Drugs fit into this model with a placebo pill acting as the “blind and controlled” portion of the study design. Food is impossible to blind (because patients and investigators can see what they eat). Diet therapy is also fraught with the fact that people’s eating behaviors are hard to regulate and analyze.
In an effort to support Dr. Swanks’ observational research, we took on the task of doing a study that fellow scientists might respect: a single-blind, randomized, controlled trial of one year’s duration. On January 15, 2009, we received approval from the ethics board of OHSU to conduct this study. Those in the intervention group were sent to the McDougall Program in Santa Rosa, CA for a 10-day education and then asked to follow the diet for a year. The raters (neurologists, radiologists, and other analysts) were “blinded” as to which patients were in the intervention (diet) group and which were in the control group (staying on the Western Diet). Over the next 4 years, 61 people were enrolled in the study. Most of the results have now been released and will soon be published in medical journals.
Important Results
 |
Permanent Compliance
Our small study has demonstrated the high compliance rate of participants with the McDougall Diet after attending the 10-day Program in Santa Rosa, CA. Total fat intake for the diet group fell to 15% of the calories consumed, and remained at this level for one year. The control group continued to consume 40% of their calories as fat. We estimate that 80% of the diet group followed the Program 100% of the time for the study period.
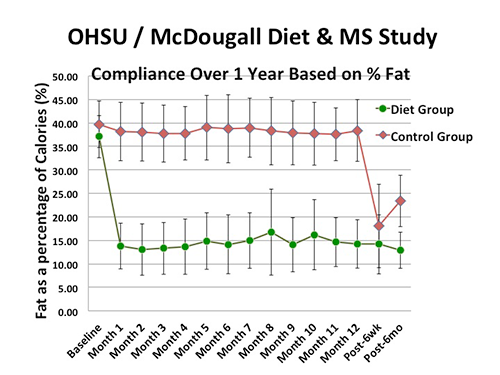 |
This finding removes one of the most common reasons given by dietitians, physicians, and other advisors for not recommending diet therapy, and that is, “No one will follow a healthy diet.” We have proven this to be folklore. Our findings are that 80% of people, properly educated, permanently change their diet.
Permanent Weight Loss
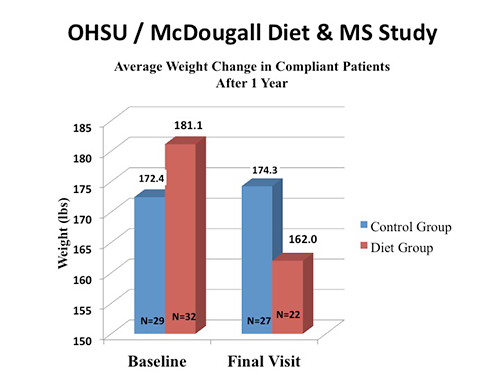 |
We also showed that people with MS who participated in the McDougall Program and followed the diet lost weight (average of 19.1 pounds) and maintained that loss for a year. Again, reflecting permanent changes. (The control group gained 1.9 pounds.)
Obesity is strongly related to the risk of developing MS, especially in children.
Multiple sclerosis is characterized by physical disability. Excess body weight is an obvious burden to activity for all people. Patients with MS should look to losing weight and improving physical fitness as a primary means to increase and maintain their function and independence.
In addition, note that these findings are from a group of younger (41 vs. 58 years) and trimmer people than the usual participants in the McDougall Program in Santa Rosa, CA. For the study, people came to us seeking help for MS, not to lose weight. Heavier individuals (as we have in our usual McDougall 10-day Programs) attain and maintain even greater reductions in weight than those observed from the Diet & MS Study.
Permanent Reductions in Blood Lipids
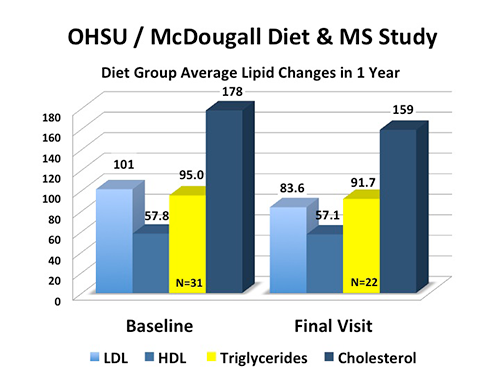 |
The diet group lowered their bad “LDL” cholesterol by 17.4 mg/dL and total cholesterol by 19.0 mg/dL. (The control group showed a 6 mg/dL reduction in both lipid measurements.) These reductions in cholesterol hold important significance for people with Multiple Sclerosis. Disease activity, as reflected by “enhancing lesions” found on MRI brain tests, is positively associated with both LDL and total cholesterol levels. Furthermore, research shows that more rapid disease progression and worsening disability is found in patients with higher LDL and total cholesterol levels. The underlying relationship between blood lipids and disease activity, disease progression, and worsening disability is due to the overall health and diet of people. (In other words, people who eat a healthy, low-fat diet have lower cholesterol and less severe multiple sclerosis because of the food.)
In addition, note that these permanent levels of cholesterol reduction are comparable to those attained by powerful statins (like Lipitor) and are achieved without the costs or side effects of drugs. Most importantly, reductions in lipids by dietary change are a result of better eating and reflect better health. Reductions in numbers attained with statins do not necessarily mean better health, and this is why real life benefits, such as fewer heart attacks and lesser chance of dying, are found to be small to imperceptible from statin therapy.
Another important finding from our study was that triglycerides did not rise when people switched to a diet high in carbohydrates. There was actually a small reduction in these lipids (95 to 91.7 mg/dL) in their blood. Some dietary “experts” have preached a false message, that carbohydrates are bad for overall health, and especially the heart, because they cause a rise in triglyceride levels. This is untrue. Triglycerides are found to go up in experiments that are rigged to show this response by requiring patients to eat more food then they naturally desire and by overfeeding them sugars and refined flours.
Permanent Reductions in Fatigue
 |
According to the Multiple Sclerosis Society, “Fatigue is one of the most common symptoms of MS, occurring in about 80 percent of people. It can significantly interfere with a person’s ability to function at home and work, and is one of the primary causes of early departure from the workforce.”
Our Diet & Multiple Sclerosis Study showed immediate and permanent positive changes in feelings of “well being” of patients with MS. Benefits for fatigue measurements were observed within a month of beginning the intervention diet and were sustained at the same improved level throughout the year. (You may relate to this benefit by remembering that endurance athletes, like marathon runners, “carbohydrate load” for energy.) The lessened fatigue may be due to a generalized reduction in inflammation resulting from less active disease. People feel better because they are healthier.
MRI Results Did Not Show Changes
The primary goal of the Diet & Multiple Sclerosis Study was to see, based on MRI images of the brain, a difference in the lesions characteristic of MS, often referred to as “plaques.” No real difference was seen between the “Diet” and “Control” groups; nor was a difference in disability or relapses seen between the diet intervention and control groups.
Although disappointing, these results were not surprising, and were realized to be the ultimate outcome from the beginning of the study, just after randomization of our small number of people (61 subjects for study). Allocating the participants, via random assignment to the diet and control group, resulted in a bias against showing positive outcomes. The diet group consisted of much sicker patients than the control group. This is seen in a higher disability score (2.72 vs. 2.22 EDSS), greater number of relapses in the previous 2 years (1.69 vs. 1.38), the higher burden of disease seen by MRI studies of the brain (4959.97 vs. 2643.26), and the greater number of newly enhancing lesions (0.78 vs. 0.11) in the diet group.
If we had been able to include 600 patients (like a typical pharmaceutical study would do), then this randomization process would have evened out the two groups making them comparable; and then (I believe) we could have seen the positive effects of a low-fat diet on these parameters of this devastating disease. Unfortunately, we could only raise about $700,000 for the study. (Pharmaceutical companies have vast financial resources to try to show benefits of their treatments.)
One year may have also been too short a time to expect meaningful MRI and clinical changes to be seen by our rather crude technologies for assessment of disease. (Even since we began our work, better imaging technology has become available.) Unfortunately follow up of this original group of 61 participants is not possible, so we’ll never know the answer to this duration question unless another study is done.
Beyond the study results, the combined work of the McDougall Program and the OHSU Neurology Department has also been a health miracle for many of the individuals who generously participated in the study (see Karen Cooper’s story).
[column col=”1/2″]
 From Dennis Bourdette, MD, Chairman of the Department of Neurology (a letter to Dr. McDougall)
From Dennis Bourdette, MD, Chairman of the Department of Neurology (a letter to Dr. McDougall)
I recently attended an international multiple sclerosis (MS) meeting in Copenhagen. Over 7,500 neurologists and researchers from Europe, North America, and other parts of the world were in attendance. This meeting, called ECTRIMS, is the premier MS research meeting that occurs each year. The most impressive thing about the meeting was the dramatic increase in interest in research on dietary and other modifiable risk factors that can increase the risk of developing MS and activate disease progression. This area of research is just getting underway but it shows a major shift in attitude. For instance, the Harvard MS group presented a paper correlating increased risk of having a MS relapse or attack with moderate to high levels of salt intake. They think salt activates the immune system. As we discussed, salt intake relates to meat, dairy, and processed food consumption and these researchers did not look into the sources of salt intake. But the key point is that such a tradition-bound research program as the Harvard group is suddenly interested in what people with MS eat! There were a number of other papers that gathered attention relating directly or indirectly to diet. So the openness of the MS research and clinical care community to look beyond genes and drugs is changing dramatically. We can and should be on the forefront of this transformation.
We also talked about the potential impact of the trial of the McDougall Diet that we completed. I think we need to celebrate the seminal nature of this study and acknowledge how it has set the stage for the future. You may recall that we encountered tremendous resistance to even doing this study. We had to address a number of concerns that the committee that approves clinical trials at OHSU had. They had concerns about the safety of the diet, the detail of your program in Santa Rosa and whether it entailed some sort of cult-like indoctrination, and the practicalities of having participants fly to Santa Rosa to learn the diet. These concerns seemed silly at the time but nonetheless we had to address them. Having gone through this process and having now successfully completed the clinical trial it will be much easier to have future studies approved by this committee.
Our study demonstrated no safety concerns and a high compliance rate of participants, and we presented the results to the scientific community at our annual neurology conference in Philadelphia in April 2014. Given the interest of the MS research and clinical care community in how obesity and vascular risk factors can accelerate disease activity over the long term, demonstrating the diet’s effects on weight and lipid, will be of great interest. Additionally, we are analyzing data on quality of life measures, insulin resistance, and some additional novel measures of lipid subtypes that may show other benefits. We will write a research paper once all of the data has been analyzed. We learnt a lot about how to conduct research on the diet and now have an important platform of data on which to build future research projects.
Finally the most impressive thing for me is how much better most people feel after they participate in your diet program. Their testimonials and enthusiasm inspire me to continue this avenue of research and clinical care. I look forward to our continuing collaboration.
With my regards,
Dennis Bourdette, MD, FANA, FAAN
Chair and Roy and Eulalia Swank Family Research Professor
Executive Director, Multiple Sclerosis Center
Oregon Health & Science University
[/column]
[column col=”1/2″]
 Vijayshree Yadav, MD
Vijayshree Yadav, MD
Principal Investigator of the Diet & MS Study
I want to thank the McDougalls for helping us do this unique diet intervention in the multiple sclerosis (MS) patients. As the principal investigator of this one year long study, I saw more than 50 people with MS experience a life changing event for them and many times their families too. I myself underwent a unique transformation in my medical practice. Although my medical school and neurology training taught me the effects of malnutrition (both under and over eating) on human health, they did not teach the idea that diet therapy alone can be curative for many of these diseases, a concept that I learnt during the close interactions with Dr. John McDougall. As a neurologist, who specializes in immunological diseases of the nervous system including MS, I had little idea that diet and lifestyle could significantly effect MS disability. Recent research in MS suggests that people with MS, who have vascular risk factors such as high blood pressure, high blood fats, diabetes, and heart disease tend to have earlier disability, as early as 6 years, than those with MS who do not have these vascular risk factors. One of the common factors for these vascular disease developments, similar to the general population, in MS is poor diet and lifestyle. Diet intervention therefore represents a significant and potentially modifiable risk factor for MS disability.
The sheer impact of preventable diseases such as heart disease and stroke (just two examples) in US is astounding. In the US, we are spending $503 billion (yes Billion, with a B!!) each year on heart disease treatment. Eighty-six million Americans (more than one fourth of our entire nation’s population) have coronary heart disease. Among these, 14 million have had a heart attack or stroke! The numbers are very scary but real!!! The number of people having new strokes each year in the US is almost 800,000 (National Heart Lung and Blood Institute data) with almost 7 million people living with a history of stroke (American Heart Association). The estimated amounts that the US spent on stroke management in 2013 ranges from $36.6 billion to $72.7 billion.
During the past 6 years while I conducted this research of diet on MS, I became increasingly aware of the vastness of the other diseases caused by poor diet. This is not just true of developed countries such as ours but the worst thing is that prevalence and incidence of poor diet and lifestyle related diseases such as heart disease, hypertension, stroke, diabetes, high blood fats, and obesity has reached epidemic proportions in the developing countries, where 5.9 billion people (out of 7.2 billion people living on planet earth) live. I was invited recently to talk about the possible role of diet and MS and other neurologic disorders at a national neurologic conference in Mumbai, India and I got to know the mammoth challenge that neurologists in India are facing as they try to tackle the “tip of the iceberg”: non-communicable diseases especially stroke. With its rapid modernization in the last 30 years, India has also witnessed a rapid increase in the preventable diseases such as diabetes, high blood lipids, obesity, hypertension, and heart disease. India harbors the world’s largest population of diabetes (more than 62 million people in 2011). The sheer knowledge of the burden of disability and death from potentially preventable diseases such as stroke was appalling to me. The number of people who suffer from stroke is much higher in the urban areas (334-424/100,000 people) but even the rural are affected not insignificantly (84-262/100,000 people). The number of people dying as a result of stroke can reach as high as 40% in some areas of India. Talking to some of the top neurologists of India, it appeared that this disease is getting out of control of the medical system in India. What was more striking to me was the lack of knowledge among the physicians about the critical role of diet in the treatment of these diseases.
The gory story is likely similar in other developing countries too as the mal effects of modernization and westernization on diet and lifestyle habits become pervasive in these societies.
I have begun to believe that the practice of medicine has to change its emphasis now to handle the mammoth problems, most of which are related to diet and lifestyle. We as physicians need better education about diet and nutrition and need to be role models to our patients. More urgently, resources need to be put into place to educate the masses.
Vijayshree Yadav, MD
Associate Professor of Neurology at OHSU Neurology and the principal investigator of the Diet and MS study
[/column]
1) Multiple Sclerosis Articles
2) Karen Cooper, Star McDougaller, from the Diet and Multiple Sclerosis Study
Recommended Articles

Giving Thanks

Mary's Mini-McDougall Diet® Q&A