Study Fails to Show Benefits of Fruits and Veggies for Breast Cancer Patients – Women are Blamed, but the Investigators Were at Fault
The meat and dairy industry must have been laughing all the way to the bank on Tuesday July 17, 2007 when headlines worldwide announced the results of a seven-year diet experiment, known as The Women’s Healthy Eating and Living (WHEL) Randomized Trial, of more than 3,000 women with breast cancer. This government funded study (kicked off by a $5 million grant from the late Wal-Mart heir John Walton with an additional $30 million in support from the National Cancer Institute) found no benefit from recommending that women with breast cancer eat more fruits and vegetables, and less fat. The chances of fewer recurrences and better survival were not seen in women previously treated for breast cancer after changes in diet achieved during this study. As a result of this paper, originally published in the Journal of the American Medical Association, more people now believe healthier eating will not help women prevent or treat breast cancer.
Incontrovertible Facts Show Women Made Few Changes
Data collected by asking the study participants about what they ate suggested they were eating more fruits and vegetables and less fat after being given instructions dictated by the study guidelines. But people don’t always tell the truth—they often want to please the investigators, so they tell them what they think they want to hear, which in this case was clearly inaccurate.
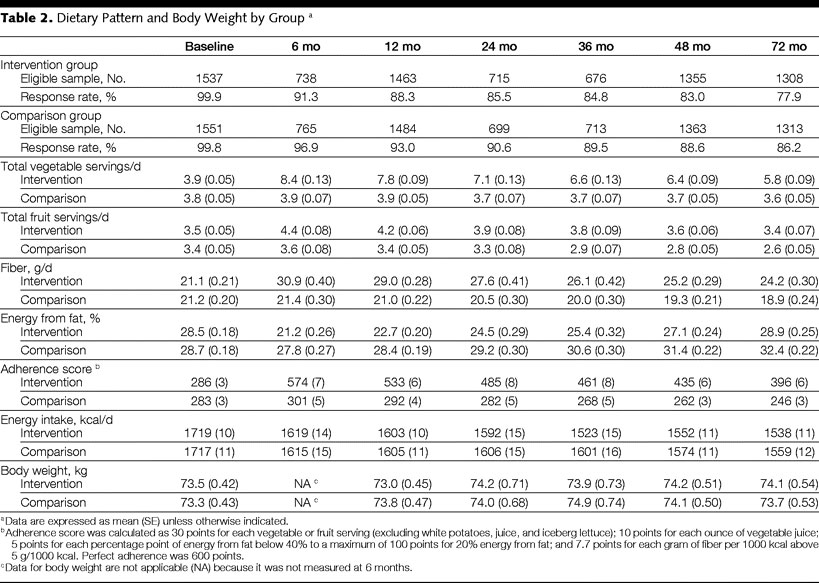
The women described as eating ‘a dietary pattern very high in vegetables, fruit, and fiber and low in fat’ did not lose any body weight at any time during the study—in fact, they gained a small amount. They were, on average, obese at 161.7 pounds (73.5 Kg) when they began the study and 6 years later they were still obese, weighing 163 pounds (74.1 Kg). (See below, table 2: Dietary Pattern and Body Weight by Group.) Nor did their average weights differ from the women who were not advised to change their diet (the control group).
Proof that the data collected from asking the women what they ate was inaccurate is shown in table 2. The women eating ‘a dietary pattern very high in vegetables, fruit, and fiber and low in fat’ were reported to have decreased their daily calorie intake by an average of 181 calories (1719 initially, and 1538 six years later), yet they gained weight. At every sixth month data collection they reported consuming at least 100 fewer calories daily than before the experiment began. A 100-calorie-plus daily deficit over a month would cause a one pound weight loss, over a year that would be 12 pounds, and over the entire 6 years of study the women should have achieved trim body weight. They gained weight!
Looking over table 2 you will also see the differences in foods consumed between the two groups were caused by the control group reporting that they ate less fruit and more fat over the study period—not by any improvement in the intervention group’s diet, other than 2 more vegetable servings a day. Yet, rather than writing about the minor absolute changes in the diet made by the intervention group, they boasted of the relative differences between the intervention and control groups—reporting impressive figures like: ‘At 4 years, relative differences in mean intake between study groups were +65% for vegetable servings, +25% for fruit servings, +30% for fiber, and −13% for energy intake from fat.
The Authors Deceived the Public
Fraud is intentional deception resulting in injury to another person. They deceived the public by claiming they were able to cause the ‘adoption of a dietary pattern very high in vegetables, fruit, and fiber and low in fat.’ Their concluding statement was, ‘during a mean 7.3-year follow-up, we found no evidence that adoption of a dietary pattern very high in vegetables, fruit, and fiber and low in fat vs a 5-a-day fruit and vegetable diet prevents breast cancer recurrence or death among women with previously treated early stage breast cancer.’ These words reflect the tone of the entire article—one of a successful experiment, not a failure—and led the public and press to believe that women in the intervention group made substantial changes in their diet. The result was headlines like: ‘No Cancer Benefit Found In Mega-Veggie-Diet Study,’ ‘Dietary Hopes Dashed for Breast Cancer Patients,’ ‘Intensive Diet Doesn’t Prevent Breast Cancer: Study,’ ‘Healthiest Diet Made Little Difference to Breast Cancer Survivors,’ and ‘Fruits, Veggies Don’t Stop Cancer Return.’ But the conscientious reader studies table 2 and correctly concludes: Even if the data reported were an accurate reflection of what these women did, two more vegetables servings a day is not a diet ‘very high in vegetables, fruit, and fiber and low in fat.’
Neither lack of intelligence nor carelessness caused the report to be written in a manner that led the public and press to incorrect conclusions; I believe the authors intentionally deceived the public. One possible motivation for distorting the truth was to save face. They wasted $35 million dollars by feeding women with breast cancer an ineffective diet. Rather than admit their mistakes, they chose to distort the real meaning of the findings of their study, and effectually, deprive women of an opportunity to become healthier by eating more fruits and vegetables.
Sixty years of scientific research, involving tens of thousands of published articles, has identified the rich Western diet as the cause of breast cancer and many scientific studies have shown that a meaningful change in diet will allow women with breast cancer to live longer and healthier. Yet, one poorly-executed, well-publicized, study may turn the tide for better health for women.
When Asked, Women Will Change
Breast cancer is a fatal disease and women will do almost anything to live. They will endure poisoning by toxic chemotherapy, burning with radiation, and mutilation from breast-amputating mastectomy; in the hopes of living a few more days. Obviously, if asked to do so, and given proper support from their doctors and dietitians, they would do something as simple, safe, cost-effective, and enjoyable as eating oatmeal and bean burritos while avoiding beefsteaks and cheese omelets. In The Women’s Healthy Eating and Living (WHEL) Randomized Trial they continued the same meat-, dairy-, oil-, and environmental chemical-laden diet that got them in trouble in the first place, with minor modifications. The investigators, not the women, should be held responsible for the fact that even the instructions to eat, ‘5 vegetable servings plus 16 oz of vegetable juice; 3 fruit servings; 30 g of fiber; and 15% to 20% of energy intake from fat,’ were followed poorly. The full cancer-inhibiting benefits of low-fat, plant-foods were never offered to these women.
A true test of diet for the prevention and treatment of breast cancer would follow the model of the diet of women worldwide who have the least chance of contracting breast cancer and the best chance of surviving it. These are women who follow a diet based on starches, like from rural Asia (rice), Africa (millet), Mexico (corn), New Guinea (sweet potatoes) and Peru (potatoes). The few women, who do get breast cancer in these societies, also live longer than their Western counterparts.
Unfortunately, a serious diet study on breast cancer is no more likely to occur than would a study on heart disease, obesity, or type-2 diabetes—diseases well accepted to be due to the Western diet. Current financial incentives are focused on maintaining the status quo. So, until the revolution against the controlling interests of big business occurs you will be left to your own means to protect yourself and your family.
Additional Note: Information The Women’s Health Initiative Randomized Controlled Dietary Modification Trial, a study also failing to show important benefits of diet for breast cancer for similar reasons, is found in my February 2006 newsletter.
Recommended Articles

The Truth About Oxalates & Kidney Stones

The Ultimate Diabetic Diet Plan: How to Manage Blood Sugar Through Nutrition







