Hormone Dependent Diseases (Male & Female)
Women’s Hormone Dependent Conditions Covered
- Abnormal Uterine Bleeding
- Early Menarche (first period)
- Fibrocystic Breast Disease
- Fibroids (tumors) of Uterus
- Late Menopause (last periods)
- Ovarian Cysts
- PMS (Premenstrual Syndrome)
Men’s Hormone Dependent Conditions Covered
- Male Pattern Baldness
- Prostate enlargement
Women are supposed to be healthy and their female organs and functions should not be “a curse”, as many women have referred to menstrual troubles for centuries. But in fact, most women do suffer considerably. You should not look for defects in the “female design” to explain the reasons for these epidemics of female troubles, but look rather to your own behavior. Men seem to have less frequent and less severe hormonal problems, in part because their sexual nature is more hidden.
Blood levels of hormones, that influence the female reproductive tissues (breasts, ovaries, and uterus) including estrogens, progesterones, and prolactin, are dependent upon your diet. A high-fat diet will increase the levels of these hormones in a woman’s body through a variety of mechanisms. Certain kinds of bacteria living normally in the colon of people who eat fatty foods, are able to convert bile acids into other substances that have hormone activity.
Another important mechanism involves recirculation of hormones. For example, estrogens, made in the ovaries and the adrenal glands, are secreted into the blood stream and then pass through the liver into the intestine. To prevent re-absorption by the intestine, these estrogens are combined in the liver with a non-absorbable substance. A high fat diet encourages growth of the bacteria in the colon that produce enzymes that uncouple those unabsorbable estrogen complexes formed in the liver. Then the uncoupled “free” estrogen is absorbed back into the blood stream, resulting in higher total levels of estrogen in the woman’s body. Fats, especially meat fats, will encourage the growth of these colon bacteria that are capable of splitting these complexes. Obviously, this means of making free-estrogens available for re-absorption can contribute to a situation that favor development of breast cancer.
Fortunately, fibers present in vegetable foods also help to block the absorption of “free” estrogens found in the bowel.
Vegetarian women, compared with those who eat meats, excrete 2 to 3 times more estrogen in their feces. Furthermore, the blood levels of certain powerful estrogens are 50% lower than are those in meat-eaters.
Obesity, too causes a body to produce more estrogens. Male hormones, called androgens, naturally present in small amounts in women, are converted to estrogens by their body fat. The more obese a woman is, the more of this conversion occurs, and the higher will be the levels of estrogen hormones from this source. The same process occurs in obese men, which is why they so often take on certain characteristics of women. Thus there are several known biochemical mechanisms by which components in the rich American diet elevate hormone levels in both men and women, to the detriment of their health.
Abnormal Uterine Bleeding:
The amount of bleeding and the severity of pain during menses are a direct consequence of the quantity of endometrial tissue, (the cells lining the inside of the uterus) that is built up each month and must be shed at the time of menstrual flow. The amount of tissue that is formed is a consequence of estrogen stimulation. A diet higher in fats means more estrogens which means more endometrial build up. Passage of large clots through the neck of the uterus during menstrual flow causes pain. Normally, menstrual blood contains factors that prevent clotting. But animal fats of the saturated type introduced in the diet cause blood to clot more readily, adding more pain to the menses.
Early Menarche:
Growing girls become women capable of reproduction at a younger age when they are raised on a high-fat diet. In most women, their first period (the menarche) begins at about the age of 12 years. On a low-fat diet the first menstrual period starts around the age of 16. A similar early maturation occurs in boys, but the effects are less dramatic. Consider the impact on girls and boys in junior and senior high school when they start expressing sexual desires four years before their mental maturity can help them to deal with adult matters. Social disharmony stirs them up, to say the least! Here’s something else for the girls to worry about; earlier onset of menstruation, not surprisingly, is associated with greater risk of developing uterus and breast cancer later on in life – a result of the longer stimulation of the vulnerable tissues by cancer-promoting estrogens.
Fibrocystic Breast Disease:
For most women breasts become tender just before the onset of their menstrual periods, when estrogen hormones reach their highest monthly levels. In approximately 10% of women the pain is described as severe. Over-stimulation of the mammary tissues by higher then normal levels of estrogens causes the breasts to swell and become tender. Eventually, after repeated bouts of inflammation the breasts develop scar tissue in many places, and some of the milk ducts become plugged, forming cysts. Fibrocystic breast disease, again not surprisingly, is associated with a higher risk of breast cancer.
Fibroids of the Uterus:
Over-stimulation of the muscle cells that make up the body of the uterus by estrogens results in the unregulated proliferation of some of these cells. The non-cancerous growth becomes a lump in the uterus. Such lumps vary in dimensions. Some rare ones have grown to the size of a basketball! These tumors do not become cancerous. The best reason for removing them is the discomfort they cause. However, for many doctors, just their presence, whether small or middle-sized, is reason enough for recommending that they be removed. After menopause, when hormone production decreases due to natural “ovary shut-down”, these fibroids soon shrink – making their owner safe both from them and from the surgeon’s knife.
Late Menopause:
Elevated levels of estrogen cause women to menstruate approximately four years longer than they would if they kept to a low-fat diet. The average age of menopause should be about 46 years, rather than 50. A prolonged menstrual life is associated with a much higher risk of breast cancer and cancer of the body of the uterus for an obvious reason: the longer stimulation of vulnerable cells by cancer-promoting estrogens.
Ovarian Cysts:
Researchers have discovered a simple alternative to fertility drugs and surgery for treating polycystic ovary disease in overweight women. Just losing weight can correct the abnormalities in the functioning of the sex hormones that are responsible for the lack of ovulation, infertility, excessive hair growth, and acne that often accompany polycystic ovaries. (Need I add that the most effective way to lose weight, and at the same time to dramatically improve the hormone balance in the body, is to adopt a low-fat, starch-based diet?)
Premenstrual Syndrome (PMS):
The cause, for obvious reasons, has been considered hormonal since the condition was first described in 1931. An estrogen-progesterone imbalance is considered to be the underlying mechanism. Because of this theory, many treatments have focused on the use of female hormone pills, especially the progesterones, for relief of the disturbance. The reason why progesterone pills work probably lies in their anti-estrogen effect. However, taking progesterone is not without undesirable side effects; it causes changes in the cholesterol in the blood, which will increase the risk of atherosclerosis and its complications, such as heart attacks and strokes. Besides, who wants to take pills everyday like a person who is always sick?
The symptoms of PMS coincide with the highest levels of female hormones in the body at during the time of the menstrual cycle. Preventing high levels of estrogens (and correcting any other hormone imbalances that may be present) is the key to dealing with PMS. And it never hurts for a woman to look better as she manages the complexities of feeling better all over.
Current Treatment
Women:
There is a better way to deal with hormone imbalance than to give hormone pills or remove the ovaries. The kinds of foods that people eat have a tremendous influence upon the hormones produced in the bodies of both men and women. Therefore, a sensible change in eating habits will lower the estrogen levels within days, and, if you’re a woman, will improve all aspects of your life that are affected by your monthly cycle. Marked benefits can be expected as soon as two months after the change in diet.
Exercise and reduction in weight in obese women can also lower their levels of estrogens. The net result from reducing the exaggerated amounts of hormones found in too many American women down to healthier levels will be better general well-being all the time and relief from troublesome signs and symptoms during menstruation. For example, painful periods and copious bleeding become lighter and less painful. I have seen the pain from a large fibroid uterus stop completely after the recommended change in diet was adopted. I would also expect that the lower hormone levels would cause the tumors to shrink, just as they do after menopause. (Studies on the relationship between fibroids and diet still must be done.) Women near menopause (the mid-forties) very often stop menstrual bleeding soon after they change their diet and start to exercise, because of the decrease in estrogens. The change to a low-fat diet has caused a reduction in breast tenderness and swelling in 60 to 100% of women afflicted with breast pains during the menstrual period.
Men:
Prostate: The prostate gland is located deep inside the pubic region and surrounds the urethra, the hollow tube in the penis through which the urine passes out of the bladder. In most men, beginning about the fifth decade of life the prostate gland will gradually enlarge. When this growth presses on the urethra, then problems with urination develop. Feeling the need for frequent urination, they need to wake up to urinate during the night, (and attendant difficulties of going back to sleep again), have difficulty getting the stream started, and dribbling during and after urination are common symptoms. Many men have enlarged prostates, and the size of the gland alone is not reason enough to submit to surgery. Only when the patient feels that these symptoms are so troublesome that his enjoyment of life is significantly affected should surgery be performed. A very rare exception to this general statement happens when the kidneys are being damaged by back pressure of the urine accumulating in the bladder. This degree of damage seldom occurs without symptoms to warn the man and his physician. Simple blood tests and X-rays will help to identify the condition in its early stages.
Sometimes, in more fortunate men, the gland enlarges in parts that do not affect the flow of urine. Sometimes, however, the enlargement will be a sign of cancer. Even so, the mere suspicion of cancer should not be used to force a patient into accepting surgery to remove the prostate gland. Usually the presence of suspected cancer is first noticed by the physician’s probing finger. And, when appropriate, the suspicion can be confirmed (or, happily, dismissed) by taking specimens at biopsy.
Long-term over stimulation of the prostate gland with male hormones, such as testosterone, is believed to be the cause of benign prostate enlargement. Higher testosterone levels are found in men who eat foods rich in fats. Malignant enlargement, caused by cancerous cells, is believed to be provoked by the same agencies.
Male Pattern Baldness:
You’re probably thinking right now that, if I blame your knife and fork for the loss of your hair, I’ve gone too far. I wouldn’t risk losing your trust if I weren’t supported by review of a Japanese book that appeared in the Journal of Dermatology, Surgery, and Oncology, titled, of all things, “Can Hair Grow Again?” The author of this book from Japan proposes that the loss of hair is the result of increased activity of sebaceous glands in the scalp that is caused by overstimulation of these glands by male hormones, testosterones. He points out an undisputed observation: a direct correlation between increased levels of animal fats (saturated fats that are eaten by males in Japan), increased levels of sebaceous gland activity in the scalps of those men, and an increased incidence of male pattern baldness in Japanese during the past 40 years. Before WW II almost every Japanese man in Japan had a full head of hair. When they move to Hawaii or California, or change their diet in Japan, as many have recently done, a number of Japanese men have become bald–just as do white and black American males.
The author of this book, Dr. Masumi Inaba, recommends treatment of male pattern baldness with a diet low in animal sources of fats and calories, accompanied by regular shampooing, and treatment of the scalp with a lotion containing an oxidizing agent to deactivate the testosterone found in the surface cells of the scalp (Minoxidil may act as an oxidizing agent). Dr. Inaba reports mild to moderate re-growth of hair in 30-50% of his cases.
Current Treatment
Men:
Prostate enlargement, like prostate cancer, is related to the levels of the sex hormones in a man’s body throughout his life. These levels are a direct consequence of the foods he chooses to eat. More specifically, a diet high in fat results in elevated levels of these hormones, and is a the primary factor in the cause of both conditions.
In general, factors that cause a disease also promote the progress of that disease. Therefore, any man with prostate cancer or simple enlargement of the gland should change his choice of foods to those that provide very little fat, in hope of gaining some benefit from the reduction of hormone levels. Certainly no harm can be done by following this recommendation.
Recently hormones which interfere with the production of testosterone have been found effective in prostatic cancer and prostatic enlargement. You should look into these investigational approaches.
Symptoms relating to frequent urination can be helped by decreasing fluid intake, especially after the evening meal. Also stop drinking caffeinated beverages, which irritate the bladder and increase the urge to urinate.
Recommendations
+-Change to a low-fat, starch-based diet. Lose excess weight (easily accomplished on this type of diet) and take moderate exercise. Avoid surgery and drugs, whenever possible.
References
+-Adlercreutz, H. Diet and plasma androgens in postmenopausal vegetarian and omnivorous women and postmenopausal women with breast cancer. Am J Clin Nutr 49:433, 1989
Woods, M. Low-fat, high-fiber diet and serum estrone sulfate in premenopausal women. Am J Clin Nutr 49:1179, 1989
Rose, D. Effect of a low-fat diet on hormone levels in women with cystic breast disease. I. Serum steroids and gonadotropins. J Natl Cancer Inst 78:623, 1987
Rose, D. Effect of a low-fat diet on hormone levels in women with cystic breast disease. II. Serum radioimmunoassayable prolactin and growth hormone and bioactive lactogenic hormones. J Natl Cancer Inst 78:627, 1987
Howie, B. Dietary and hormonal interrelationships among vegetarian Seventh-Day Adventists and nonvegetarian men. Am J Clin Nutr 42:127, 1985
Hill, P. Plasma hormones and lipids in men at different risk of coronary artery disese. Am J Clin Nutr 33:1010, 1980
Hill, P. Diet, lifestyle and menstrual activity. Am J Clin Nutr 33:1192, 1980
Hill, P. Diet and prolactin release. Lancet 2:806, 1976
Hamalainen, E. Diet and serum sex hormones in healthy men. J Steroid Biochem 20:459, 1984
Ingram, D. Effect of low-fat diet on female sex hormone levels. J Natl Cancer Inst 79:1225, 1987
Gorbach, S. Estrogens, breast cancer, and intestinal flora. Rev Infect Dis 6(suppl 1):S85, 1984
Goldin, B. Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women. N Engl J Med 307:1542, 1982
Goldin, B. Effect of diet on excretion of estrogens in pre- and postmenopausal women. Ca Res 41:3771, 1981
Boyd, N. Effect of a low-fat high-carbohydrate diet on symptoms of cyclical mastopathy. Lancet 2:128, 1988
Aksel, S. Etiology and treatment of dysfunctional uterine bleeding. Obstet Gynecol 44:1, 1974
Baird, D. Medical management of fibroids. Br Med J 296:1684, 1988
McKenna, T. Pathogenesis and treatment of polycystic ovary syndrome. N Engl J Med 318:558, 1988
Polson, D. Polycystic ovaries–a common finding in normal women. Lancet 1:870, 1988
Abraham, G. Nutritional factors in the etiology of the premenstrual tension syndromes. J Reprod Med 28:446, 1983
Prior, J. Conditioning exercise decreases premenstrual symptoms: a prospective, controlled 6-month trial. Fertil Steril 47:402, 1987
Vaitukaitis, J. Premenstrual syndrome. N Engl J Med 311:1371, 1984
Sanchez, A. A hypothesis on the etiological role of diet on the age of menarche. Med Hypotheses 7:1339, 1981
Schwartz, S. Dietary influences on the growth and sexual maturation in premenarchial rhesus monkeys. Horm Behav 22:231, 1988
Inaba, M. Can Human Hair Grow Again? J Dermatol Surg Oncol 12:672, 1986
Wilson, J. The pathogenesis of benign prostatic hypertrophy (review). Am J Med 68:745, 1980
Hill, P. Environmental factors and breast and prostate cancer. Ca Res 41:3817, 1981
Johansson, J. Natural history of localized prostatic cancer. A population-based study in 223 untreated patients. Lancet 1:799, 1989
Editorial–Running, jumping, and…amenorrhoea. Lancet 2:638, 1982
Ding, J. High serum cortisol levels in exercise-associated amenorrhea. Ann Intern Med 108:530, 1988
Recommended Articles
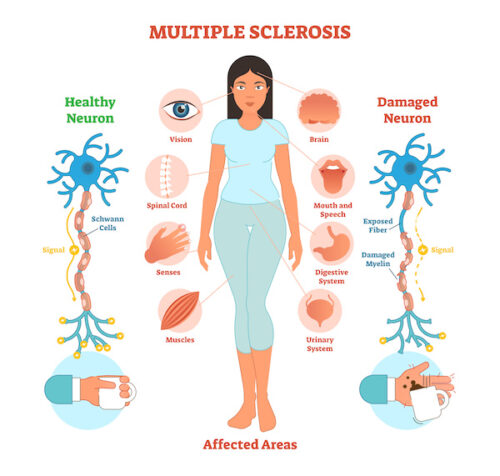
Multiple Sclerosis (MS) & Diet

Salt: The Scapegoat for the Western Diet






