The Angioplasty Debacle
This article originally appeared in the September 2006 McDougall Newsletter and has been updated in January 2023.
By John McDougall, MD
With heart disease you face the biggest of all the medical businesses. In 2001, in the United States, more than one million coronary angioplasty procedures were performed at a cost of more than $30 billion, and more than 500,000 coronary bypass operations were performed at a cost of another $30 billion.1 Assume that your local general hospital derives 80% of its income from heart disease. The average total healthcare cost after three years is $63,896 for angioplasty (compared to $84,364 for bypass surgery).2 You had best be prepared for some high-pressure sales when you become involved with heart surgery—and take all the necessary time to be sure you are making a wise purchase. My experience has been most patients are misinformed by their doctors about the real benefits and harms of the treatments offered—and all that money plays a big part in the dishonesty.
The Angioplasty Procedure
Angioplasty is a surgical procedure used to open blockages caused by atherosclerosis in the arteries, most commonly in the heart arteries. The most descriptive name used for this treatment is: Percutaneous (through the skin) transluminal (inside the blood vessel) coronary (relating to the heart) angioplasty (blood vessel repair). When a stent is also used the procedure is called a Percutaneous Coronary Intervention (PCI). The stent is a tiny wire mesh tube used to help keep the treated artery open after the initial angioplasty. About 90 percent of angioplasty procedures these days include the use of a stent.
Terms Used for Angioplasty:
Balloon angioplasty
Coronary angioplasty
Coronary artery angioplasty
Cardiac angioplasty
Percutaneous transluminal coronary angioplasty
PTCA
Heart artery dilatation
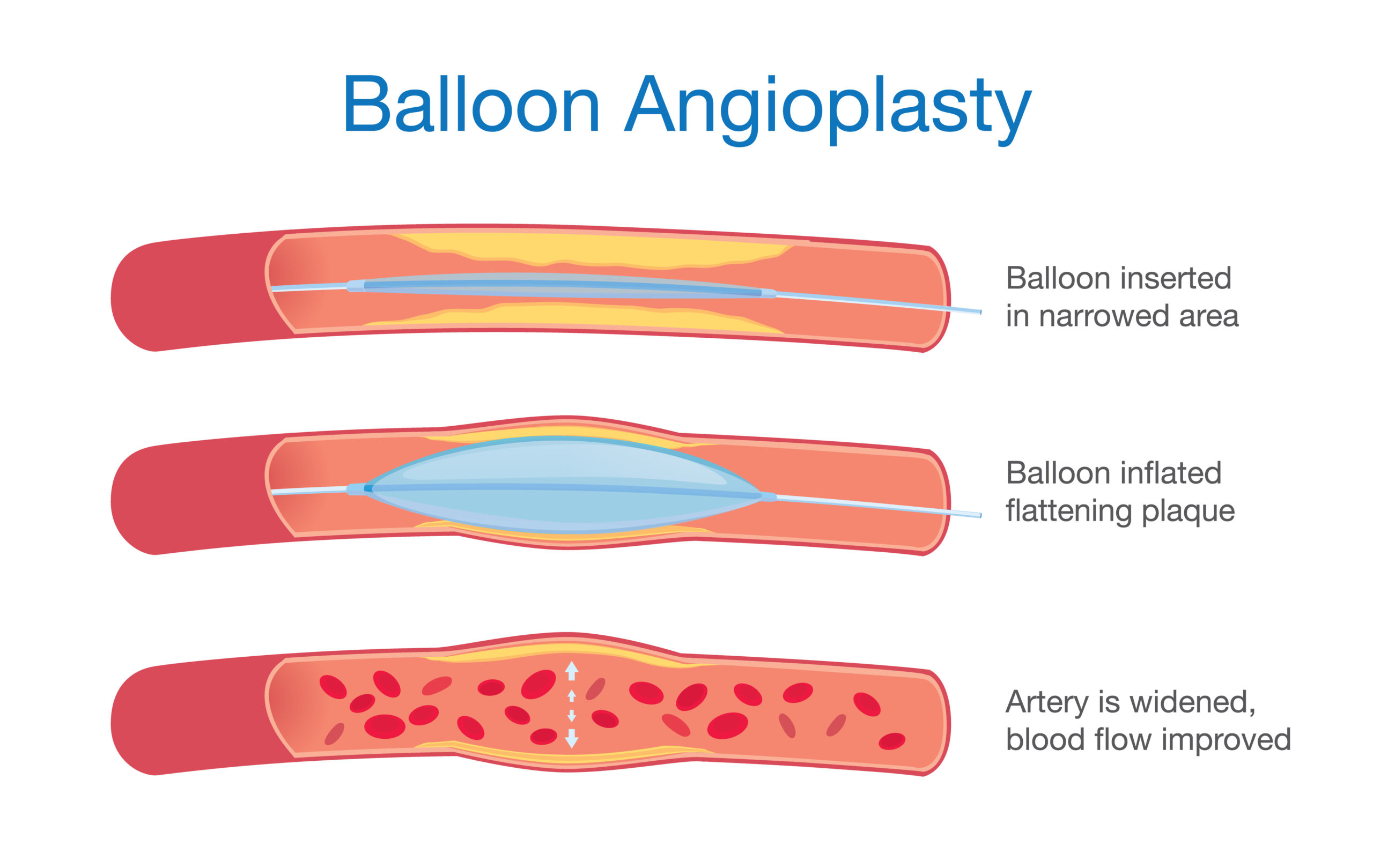
During the procedure a catheter with a guidewire is placed in the femoral artery of the leg, near the groin, or a main artery in the arm. Using x-rays, the catheter is fed up into the heart (coronary) arteries. Dye is then injected in order to visualize shadows of the inner artery lumen. When a narrowed segment is identified a balloon-tipped catheter is passed into this area and inflated. The balloon compresses the plaque that is causing the narrowed area, squashing it outwardly against the arterial walls.
A stent is next placed over a catheter and inserted into the area that has been compressed during the angioplasty procedure. When the balloon is inflated again, the stent expands and stays permanently in place.
Angioplasty Does Not Save Lives
Although angioplasty has been performed for nearly 3 decades and over one million procedures are done annually, you should be astonished to learn this fact: Angioplasty has never been shown to save the lives of patients who are treated for chronic heart blockages.3,4 I know this statement defies logic. After all, the skilled surgeon has just dilated a stricture in your heart artery.
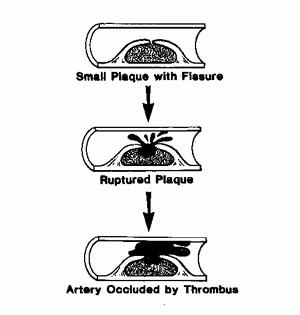
To understand why this procedure does not save lives, you need to learn how a heart attack occurs. All doctors know, and all patients need to realize, that a heart attack occurs when a small volatile plaque, better pictured as a tiny festering sore, located on the inside of an artery ruptures and causes the blood to suddenly form a clot (thrombus).5,6 The clotting occurs as a result of the release of “products of injury” when the sore ruptures—similar to the clot that forms when you cut your hand—except this clot often fills the blood vessel. The event of blood clot formation in the heart artery is known as a coronary artery thrombosis, or heart attack. The reason lives are not saved by angioplasty is this treatment completely ignores the dangerous part of the artery disease, the volatile plaques (sores). Instead the doctor’s efforts are directed toward dilating a narrowing caused by a large, stable, fibrous, plaque—this latent stage of artery disease almost never ruptures and therefore does not lead to a heart attack when left alone. However, when the plaque is ruptured by angioplasty surgery, heart attacks occur in 3 to 5% of patients.7
Half the Arteries Operated on Close down within Five Months7
A potentially devastating result from the injury caused to the artery wall by angioplasty is blood clot formation and closure of the treated artery. This should not be surprising. When the plaque is ruptured by the expanding balloon, “products of injury” are released—as expected, these substances cause the blood to clot within the artery. Within five months of the surgery up to 50% of arteries treated by angioplasty are completely closed down.7 This is common knowledge among doctors, therefore many efforts have been made to reduce this complication, including the use of blood thinning agents, such as aspirin, Plavix, fish oil and heparin before and after surgery. The benefits from these medications have been limited. The next effort to stop postsurgery artery closure has been the use of mechanical devices, called stents, which prop the artery open.
Stents, a Temporary Solution
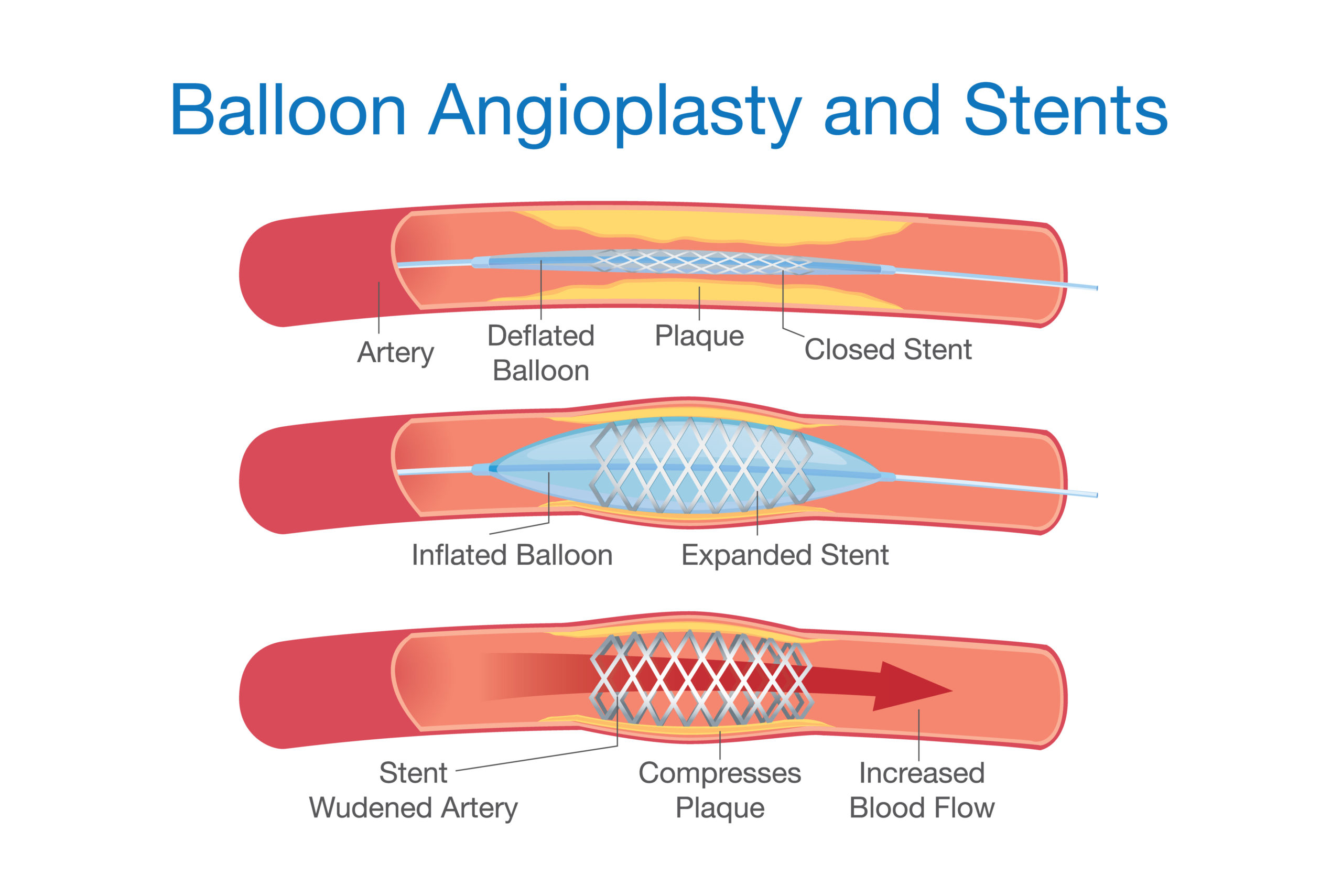
Since the mid 1990s wire mesh stents have become a standard part of the angioplasty procedure. Unfortunately, these wire cylinders (stents) irritate the smooth muscle cells of the artery walls causing these cells to grow aggressively (to proliferate). This growth is an effort by the body to cover up the foreign metal that has just been introduced into the artery by the surgeon. This should not be surprising. Whenever an irritating alien material is placed in the body, cells grow around it in order to isolate the unfamiliar substance, which the body perceives as potentially harmful. The growth of the muscle cells (and blood clots) eventually closes 20% to 41% of the arteries containing these metal mesh stents.8 Furthermore, the use of stents results in no better survival than angioplasty alone7,9—and remember angioplasty does not improve the chances of living longer.3,4 If only treatments could be developed to stop these cells from growing. Scientists had to look no further than cancer therapy to find tools to stop cells from proliferating.
Brachytherapy, Stop Proliferation with Radiation
Radiation kills cells and stops them from proliferating—a treatment used for decades to stop cancer cells from growing. Brachytherapy is the use of radioactive seeds placed after angioplasty through the catheter to the site of balloon treatment. The seeds stay in place for about 20 to 45 minutes, and then the catheter is removed. Brachytherapy is effective in preventing in-stent closure (restenosis) by stopping the proliferation of blood vessel smooth muscle cells, and associated scar tissue. Unfortunately, the early benefits of this therapy were not sustained, and the injury to the arteries caused by the radiation encourages the formation of blood clots that occlude the arteries and cause death.
The long term follow up of patients treated with this procedure has shown an unacceptable high rate of major adverse cardiac events despite prolonged administration of combined therapy with blood thinning (antiplatelet) drugs.10 The adverse events are mainly due to blood clot formation and artery closure. This closure usually occurs during the first year after brachytherapy. In one recently reported study 38% of people suffered life-threatening episodes and 53% had to be reoperated on within 5 years.11 As a result, the two companies that made brachytherapy devices removed their machines from the market.
Drug Eluting Stents, Stop Proliferation with Chemotherapy
Placing a coating of cancer drugs onto the stents is now the most popular method used to inhibit the proliferation of smooth muscles cells after angioplasty. Two kinds of stents are available: the sirolimus-eluting (Cypher) and the paclitaxel-eluting (Taxus). Around 6 million people so far have drug eluting stents in their heart arteries. The restenosis rate was zero at six months after placement of the drug eluting stent compared to 26% after the bare metal stent.12 But at one year there was no difference in deaths or heart attacks between the drug-eluting stents and the bare metal ones.13,14 However, four years later the results are disturbing. Two recent studies showed the risk of death and heart attacks are higher with the drug-eluting stents compared to the bare metal, uncoated stents.15
Mandatory Blood Thinners Post-Op for Life
Because of the high risk of artery closure (restenosis) from blood clotting after an angioplasty with or without a stent, blood thinners have been routinely prescribed. A baby aspirin daily has been the time honored treatment to prevent the formation of clots in the arteries—this drug is relatively safe and effective. To aspirin has been added another class of blood thinner drugs called thienopyridine—these include Plavix (clopidogrel) and Ticlid (ticlopidine). When combined with aspirin, there is a high risk of bleeding from this class of drugs.16
The risk of blood clot formation after a bare metal stent decreases after 2 to 4 weeks as the smooth muscles cells cover the bare metal.17 Because the drug-eluting stents delay coverage of the stent by proliferating cells, the risk of blood clotting is prolonged. Until recently, recommendations were to use a drug like Plavix for a minimum of 3 to 6 months after surgery in addition to lifelong aspirin therapy.17 Recent reports of sudden death months and years after the placement of drug-eluting stents has caused doctors to rethink the time someone should be taking these medications.17 The truth is they really don’t know what to do—so, doctors, running scared from fear of law suits, are now recommending that patients who have these kinds of stents should be on aspirin and a Plavix-like drug for life.
What Would I Do?
I have studied heart disease for the past 35 years, and everything I know about angioplasties and bypass surgery makes me want to stay clear of these businesses unless there is absolutely no other alternative. The real alternative that too few people take advantage of is prevention: A low-fat, plant-food based diet, exercise, and clean habits will prevent this disease. Once the disease has started it can be stopped and in most cases reversed with this lifestyle medicine.18
The only indication for angioplasty is to relieve incapacitating chest pain—since this surgery has not been shown to save lives.3,4,7,9,13,14 To use the promise of prolonging lives as the sales pitch is dishonest.
If I had incapacitating chest pain I would have an angioplasty. The key word here is incapacitating. f I got chest pains while climbing to the top of a mountain, I would not have surgery—I would just give up climbing because I do not care for this kind of activity. However, if I had chest pains so severe that they kept me from riding my windsurfer across the bay, I would have surgery—because, for me, this limitation would be incapacitating. Of course, before agreeing to surgery I would change my diet; this change alone has been shown to reduce chest pain episodes by 90% in 3 weeks19 and I would consider medications known to relieve chest pains—medications like nitrates (nitroglycerin) and beta blockers. I would also use enough cholesterol-lowering medication to lower my levels to below 150 mg/dl. (See Cleaning Out Your Arteries.)
My first surgical attempt to reduce the blockage that is causing my heart to hurt would be with a standard angioplasty, no stent. If that procedure failed then my next effort would be the use of a bare metal (uncoated) stent. After surgery, I would take aspirin and Plavix for one month, and then stop the Plavix, but continue one baby aspirin a day for life.
I am sure situations exist that would cause me to elect bypass surgery if the angioplasty failed, fortunately, I cannot think of any right now. The indications for bypass surgery are:
1) Incapacitating chest pain
2) Damage to the left ventricle (heart chamber) causing 50% or less of the blood to be ejected from the heart with each beat (ejection fraction). For these patients there is an 18% survival advantage with surgery over 10 years.20 For me, this small benefit would not cause me to rush into the operating room.
Hopefully, you will never become involved in the heart disease businesses—you can’t win here. If you do, then you must make every effort to become a well-informed consumer and a very “squeaky wheel” by asking questions and getting complete scientifically backed answers, until you are fully satisfied that this is your best choice. My educated guess is that over 95% of angioplasty and bypass surgeries could be avoided if proper medical indications were adhered to, patients were fully informed of the limitations and hazards, and every patient took full advantage of the powerful healing which can be effected by a change to a low-fat, plant-food based diet and by commitment to exercise.
References:
1) One million angioplasty surgeries in 2001: http://appropriations.senate.gov/hearmarkups/record.cfm?id=224132
2) Stroupe KT, Morrison DA, Hlatky MA, Barnett PG, Cao L, Lyttle C, Hynes DM, Henderson WG; Investigators of Veterans Affairs Cooperative Studies Program #385 (AWESOME: Angina With Extremely Serious Operative Mortality Evaluation). Cost-effectiveness of coronary artery bypass grafts versus percutaneous coronary intervention for revascularization of high-risk patients. Circulation. 2006 Sep 19;114(12):1251-7.
3) No Authors. Coronary angioplasty versus medical therapy for angina: the second Randomised Intervention Treatment of Angina (RITA-2) trial. RITA-2 trial participants. Lancet. 1997 Aug 16;350(9076):461-8.
4) Henderson RA, Pocock SJ, Clayton TC, Knight R, Fox KA, Julian DG, Chamberlain DA; Second Randomized Intervention Treatment of Angina (RITA-2) Trial Participants. Seven-year outcome in the RITA-2 trial: coronary angioplasty versus medical therapy. J Am Coll Cardiol. 2003 Oct 1;42(7):1161-70.
5) Fuster V, Moreno PR, Fayad ZA, Corti R, Badimon JJ. Atherothrombosis and high-risk plaque: part I: evolving concepts. J Am Coll Cardiol. 2005 Sep 20;46(6):937-54.
6) Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006 Apr 18;47(8 Suppl):C13-8.
7) Nordmann AJ, Hengstler P, Harr T, Young J, Bucher HC Clinical outcomes of primary stenting versus balloon angioplasty in patients with myocardial infarction: a meta-analysis of randomized controlled trials. Am J Med. 2004 Feb 15;116(4):253-62.
8) Suttorp MJ, Laarman GJ, Rahel BM, Kelder JC, Bosschaert MA, Kiemeneij F, Ten Berg JM, Bal ET, Rensing BJ, Eefting FD, Mast EG. Primary Stenting of Totally Occluded Native Coronary Arteries II (PRISON II): a randomized comparison of bare metal stent implantation with sirolimus-eluting stent implantation for the treatment of total coronary occlusions. Circulation. 2006 Aug 29;114(9):921-8.
9) Zhu MM, Feit A, Chadow H, Alam M, Kwan T, Clark LT. Primary stent implantation compared with primary balloon angioplasty for acute myocardial infarction: a meta-analysis of randomized clinical trials. Am J Cardiol. 2001 Aug 1;88(3):297-301.
10) Nikas DN, Kalef-Ezra J, Katsouras CS, Tsekeris P, Bozios G, Pappas C, Naka KK, Kotsia A, Papamichael N, Sideris DA, Michalis LK. Long-term clinical outcome of patients treated with beta-brachytherapy in routine clinical practice. Int J Cardiol. 2006 Aug 2;
11) Steve Sternberg, USA Today: http://www.usatoday.com/news/health/2004-09-30-heart-usat_x.htm
12) Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, Colombo A, Schuler G, Barragan P, Guagliumi G, Molnar F, alotico R; RAVEL Study Group. Randomized Study with the Sirolimus-Coated Bx Velocity Balloon-Expandable Stent in the Treatment of Patients with de Novo Native Coronary Artery Lesions. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002 Jun 6;346(23):1773-80.
13) Spaulding C, Henry P, Teiger E, Beatt K, Bramucci E, Carrie D, Slama MS, Merkely B, Erglis A, Margheri M, Varenne O, Cebrian A, Stoll HP, Snead DB, Bode C; TYPHOON Investigators.Sirolimus-eluting versus uncoated stents in acute myocardial infarction. N Engl J Med. 2006 Sep 14;355(11):1093-104.
14) Laarman GJ, Suttorp MJ, Dirksen MT, van Heerebeek L, Kiemeneij F, Slagboom T, van der Wieken LR, Tijssen JG, Rensing BJ, Patterson M.Paclitaxel-eluting versus uncoated stents in primary percutaneous coronary intervention. N Engl J Med. 2006 Sep 14;355(11):1105-13.
15) Hitchen L. Mortality is higher with drug eluting stents than with uncoated stents, studies find. BMJ. 2006 Sep 16;333(7568):569.
16) Diener HC, Bogousslavsky J, Brass LM, Cimminiello C, Csiba L, Kaste M, Leys D, Matias-Guiu J, Rupprecht HJ; MATCH investigators. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet. 2004 Jul 24;364(9431):331-7.
17) Spertus JA, Kettelkamp R, Vance C, Decker C, Jones PG, Rumsfeld JS, Messenger JC, Khanal S, Peterson ED, Bach RG, Krumholz HM, Cohen DJ. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation. 2006 Jun 20;113(24):2803-9.
18) Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, Ports TA, McLanahan SM, Kirkeeide RL, Brand RJ, Gould KL. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990 Jul 21;336(8708):129-33.
19) Ornish D, Scherwitz LW, Doody RS, Kesten D, McLanahan SM, Brown SE, DePuey E, Sonnemaker R, Haynes C, Lester J, McAllister GK, Hall RJ, Burdine JA, Gotto AM Jr. Effects of stress management training and dietary changes in treating ischemic heart disease. JAMA. 1983 Jan 7;249(1):54-9.
20) Alderman EL, Bourassa MG, Cohen LS, Davis KB, Kaiser GG, Killip T, Mock MB, Pettinger M, Robertson TL. Ten-year follow-up of survival and myocardial infarction in the randomized Coronary Artery Surgery Study. Circulation. 1990 Nov;82(5):1629-46.
Recommended Articles
Arsenic In Rice

Finding a Healthcare Provider






