Common Health Problems: Colitis (Mild and/or Non-specific), Irritable Bowel Syndrome, Spastic Colitis
The contents of the large bowel are the primary determinant of the health and function of the intestine, and a spastic colon is no exception to this rule. Few physicians have even an elementary understanding of the influence that foods can have on the body: they are unprepared to deal with health and disease from this fundamental perspective.
Possibly it is too simple and obvious a fact that the contents of the large intestine will determine whether or not the stool will be large or small, hard or soft, and if defecation will be painful or not, and whether or not blood and mucus will accompany passage of the stool. (This is a clear case of not seeing the forest for the trees.) Could the fear that the very foods the physicians and dietitians themselves eat and feed to their families can also be the cause of their patient’s illness be too personal a threat for most health professionals? The “high-tech” drug solution would be much more easy to accept for most men and women of science.
The correct stool contents that make a healthy colon are the remnants of the foods after the digestive processes have acted upon foods high in fibers and low in fats, and devoid of all animal components (especially dairy products). Fibers will actually sooth the irritated bowel. Contrary to popular conception, fibers are not coarse scratchy strands of plant materials, like the bristles in a broom. Fiber is a general term used to describe long complex chains of sugar molecules that are attached by linkages that resist normal digestion by enzymes in the human small intestine, and therefore end up more or less intact in the large bowel. The intestinal bacteria in the colon do have the capacity to break down some of the linkages in those fibers. These microscopic remnants of fibers are soft, not irritating to the intestinal lining, and will absorb water to help form a soft stool that still has considerable bulk.
Most people with irritable bowel syndrome improve almost as soon as they begin to eat a starch-based diet that provides all types of fresh or fresh-frozen plant foods.
Recommendations
+-Don’t you take the blame for having this disease. The cause is not stress, nor “tranquilizer deficiency.” Your bowel problems are not due to your emotional make up (although unending bowel pains and diarrhea can drive even the strongest person to emotional collapse). Rather you should focus your attention on the contents of your intestine. A starch-centered diet brings almost overnight relief for this “psychological” disease.
You should also eat plenty of these good foods at first, in order to fill up that lower intestine with the right stuff quickly. However, an occasional sufferer will need to avoid the specific plant foods that may be causing an allergic reaction. Foods from the plant kingdom that are notorious for inducing “allergic-type” reactions are wheat and citrus fruits, and they should be avoided initially when trying to end bowel distress. As a final step toward resolving a difficult case of irritable bowel syndrome, the Elimination Diet should be followed. (See Allergic Reactions to Food for explanation of this elimination diet.) Some patients may need medication to control symptoms when first starting this diet.
If your colitis is triggered by “hot spices” such as Mexican salsa or Indian curries then the solution is obvious–eliminate these irritants.
References
+-Danivat, D. Prevalence of irritable bowel syndrome in a non-Western population. Br Med J 296:1710, 1988
Harvey, R. Prognosis in the irritable bowel syndrome: a 5-year prospective study. Lancet 1:963, 1987
Sullivan, S. Management of the irritable bowel syndrome: a personal view. J Clin Gastroenterol 5:499, 1983
Bentley, S. Food hypersensitivity in irritable bowel syndrome. Lancet 2:295, 1983
Jones, V. Food intolerance: a major factor in the pathogenesis of irritable bowel syndrome. Lancet 2:1115, 1982
Childs, P. A new look at diarrhea, diverticulitis and `colitis’ after 25 years of clinical study. Practitioner 215:757, 1975
Recommended Articles
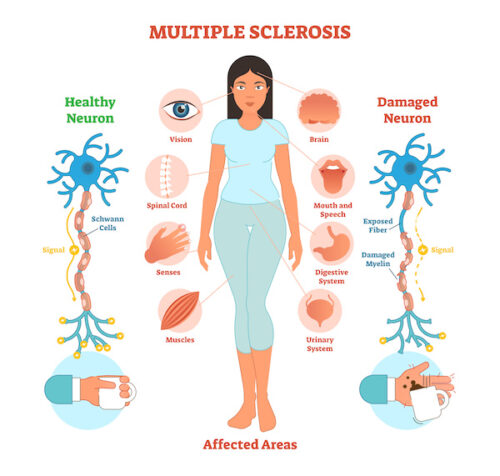
Common Health Problems: Multiple Sclerosis (MS) & Diet

Is Falling Asleep After Eating a Sign of Diabetes?






